Case Background
A 45-year-old male patient has previously presented to our office in 2015 with the chief complaint of having a hole in the back of his right maxillary central incisor (Figure A). The patient stated he had trauma to the tooth at age 18 and that the tooth was repositioned by a dentist.

The patient had endodontic treatment started on tooth #8 six years prior to that visit, but never returned for completion. The temporary restoration dislodging from the palatal aspect of the tooth prompted the patient to come in for treatment. Cotton was present in the canal (Figure B).

Initial Diagnostics and Treatment
Periapical radiographs of # 8 were taken and other than slight discoloration and a minor facial swelling, no discomfort was reported. A gingival abscess was traced to mid-level of tooth radiographically (Figure C).

At this point, the endodontic procedure for tooth # 8 was completed up to the point where we believed the root to end (Figure D) noting that there was a possible fracture further apical to that point. A lingual composite was placed on # 8. The patient was made aware that the prognosis for the tooth was guarded.

The patient did not return for the subsequent follow-up appointment that was scheduled. Additional attempts to get the patient to return in the following year were unsuccessful.
Six Years Later
Six years after the initial visit, in February of 2022, the patient returned with the chief complaint of, “My front tooth is painful, it moves, it is discolored, and sometimes it has an abscess”. The examination revealed that tooth #8 had grade three mobility, with suppuration emanating from the sulcus upon palpation of the gingiva. The periapical radiograph showed resorption of the root at the point where the gutta percha fill of the root canal treatment ended (Figure E).

The apical fracture of #8 was more clearly noted in this image. The apical portion seemed ankylosed. The initial assessment based on the 2D images was to extract and evaluate for a bone graft/membrane placement, allow three to four months of healing time, and then reassess for implant placement. The patient inquired if there was any chance for the implant to be placed at the time of extraction and if the fractured part of the root would be removed.
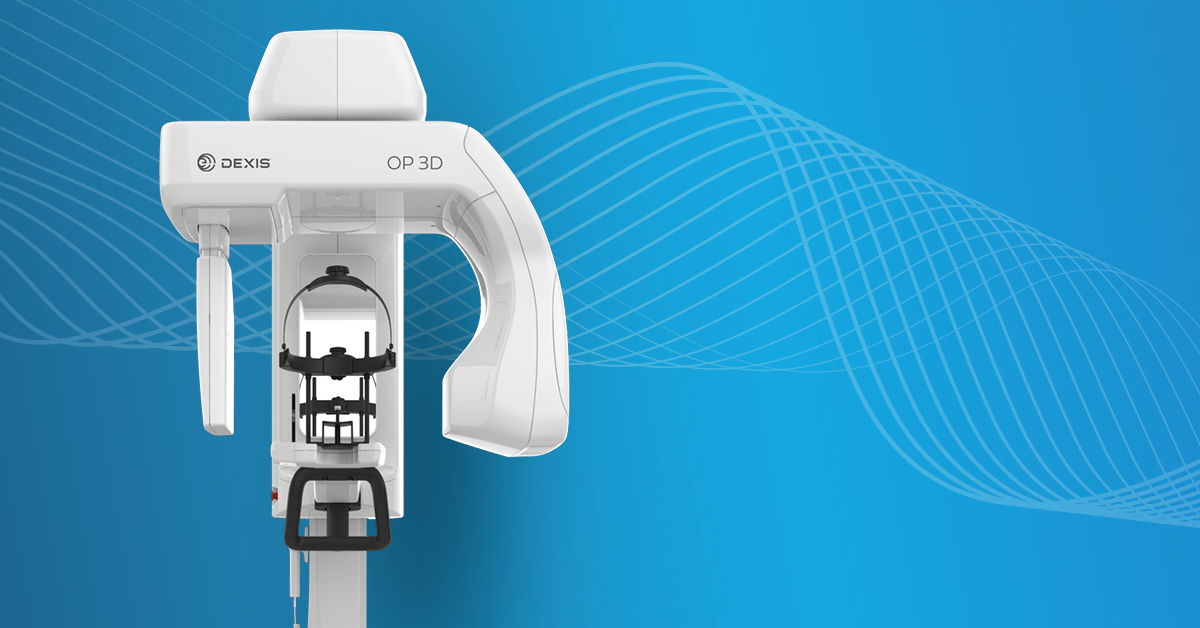
3D Visualization
3D imaging was used to determine the appropriate treatment plan. A DEXIS OP 3D 5×5 cm FOV with the endodontic resolution protocol (95 kVp, 2mA, 80 μm) was taken to see the bone pattern and periodontal ligament space surrounding the damaged tooth. We were able to visualize the true size of the apical fracture for tooth # 8, as well as the full dimensions of the bone (Figure F).

3D visualization enabled me to see not only the broken apical aspect of the tooth but also a small breakaway of a piece of the root nearing the palate in the cross-sectional view (Figure G).

This greater diagnostic power allows me show my patients what is going on under the surface; ultimately resulting in acceptance of the treatment plan (Figure H).

Treatment Planning in 3D
3D imaging data provides a level of clarity beyond the limitations of 2D intra and extra-oral imaging. It allows us to assess if the quality and quantity of bone was viable for dental implant placement. With the ability to view the patient’s #8 in three dimensions, we were able to make several definitive diagnoses. The apical fracture is sizeable, but it does not appear to be as ankylosed as I originally hypothesized. The suppuration appeared to emanate from the mid root area, with no visible pathology around the apical fracture of the root (Figure I). As a result, we proposed immediate placement of an implant in the site at #8.

If we are successful in removing the root tip in an atraumatic fashion and can debride the area of all infectious tissue and place an immediate implant. Once accomplished, we would create a temporary using the coronal portion of patient’s existing tooth and apply a lingual splint that would bond the coronal of #8 to the adjacent teeth (the patient has a class III bite). After three to four months of osseointegration, restoration for #8 would commence.
Conclusion
In this clinical case, although the apical fracture of #8 was seen on the 2D x-rays, the DEXIS OP 3D gave diagnostic clarity on the patient’s failing tooth.
The patient was unsure about how to proceed, but after reviewing the scan and discussing the possibility of immediate placement of an implant, the patient agreed to move forward with the treatment plan.
If we are indeed able to perform immediate placement, this technique would allow for a streamlined surgical experience, a shorter treatment time and reduced time with the temporary tooth by months.
Learn more about DEXIS OP 3D and how it can address your advanced dental imaging needs here: https://www.pattersondental.com/equipment-technology/digital-imaging/extraoral/dexis-op-3d
About Dr. Gaur
 Dr. Raj Gaur attended Binghamton University, where he received a Bachelor of Science degree in Biology. After graduating from the New Jersey Dental School at the University of Medicine and Dentistry, Dr. Gaur enrolled in a General Dental Residency program at Jamaica Hospital Medical Center in Jamaica, New York.
Dr. Raj Gaur attended Binghamton University, where he received a Bachelor of Science degree in Biology. After graduating from the New Jersey Dental School at the University of Medicine and Dentistry, Dr. Gaur enrolled in a General Dental Residency program at Jamaica Hospital Medical Center in Jamaica, New York.
Dr. Gaur began private practice in the Triboro area of New York in 2007. In 2012, he purchased a private practice on Long Island, which now serves as a general and pediatric dentistry office.
While not at work, Dr. Gaur enjoys maintaining an active lifestyle, traveling and spending time with his wife and three children.



You must be logged in to post a comment.